Cuba is ranked as a Third World country, but the education and health systems are equivalent to or better than those of all First World countries.
The infant mortality rate is 4.7 per 1000 births (equivalent to Canada, the USA and Australia), life expectancy is 78 years, and the literacy rate is 99.8% of adults over 15 years (the highest in the world). In 1960 the infant mortality rate was 60/1000 births and life expectancy was 60 years.
Despite being under an embargo from the USA since the revolution, which stopped all imports from the big pharmaceutical companies, Cuba has eradicated 14 infectious diseases, including malaria, from its population.
Legacy of inequality
Prior to the 1959 revolution, Cuba’s health care system was based on the US and French models, with well-trained doctors but an inequitable distribution of care. Between 1959 and 1967, almost half of those doctors left Cuba, mainly for the United States. In 1960 only 11.2% of farm worker families drank milk and only 2% were eating eggs; rural medical services were virtually non-existent.
The revolutionary government of Fidel Castro defined health and education as social responsibilities of government and individual rights of citizens. Doctors at the helm of the revolutionary government’s health initiatives took bold steps to recruit doctors for the Rural Health Service, setting up 50 new rural hospitals, establishing more than 160 community clinics in urban areas and initiating the national children’s immunisation program, while training many health professionals.
In the ’70s, the first investments were made in new general hospitals and pharmaceutical production plants. The community clinic (“polyclinic”) model of primary health care was reinforced and expanded, taking on health education, prevention and environmental monitoring. Maternal and child health, from the start a priority for the new health system, evolved into the first national comprehensive health program; it was later joined by three more: infectious diseases, chronic diseases and the elderly. As the numbers of medical graduates rose, more Cuban health professionals joined international service abroad to provide free medical services, primarily in the nations of Africa and Latin America. By the end of the next decade, the cumulative record showed Cuba had posted nearly 20,000 health professionals abroad. (In our own region, Cuba has had an ongoing involvement with training doctors in East Timor).
The ’80s were also the decade for two decisive developments that became hallmarks of Cuban medicine. The first was the take-off of the biotechnology industry, which would put Cuba in the forefront of global vaccine research (e.g., the first vaccine against Haemophillus influensae type b was made in Cuba, even though the capitalist world recognised only the Swedish discovery!). The second was the introduction of the Family Doctor Program in 1986, which located doctor-and-nurse teams literally next door to their patients. By the early ’90s, more than 95% of Cuban families would receive primary medical attention in their own neighbourhoods.
Overcoming economic crisis
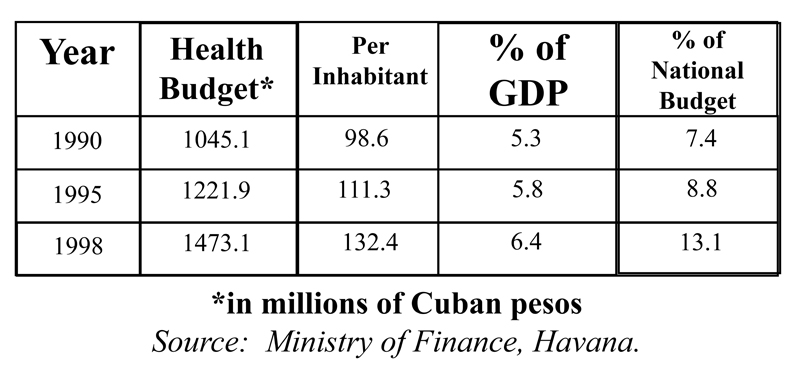
The collapse of the Soviet Union and the “Eastern bloc” affected Cuba in many ways. The island lost 85% of its trade, threatening the economy and the health system with collapse. The “Cuban Democracy Act” (Helms Burton) in the US in 1992 tightened the US embargo. The remarkable fact is that – with the exception of a 1992-93 neuropathy epidemic – infant mortality was 10.7 per 1000 live births in 1990, down to 9.4 by 1995 and to 7.2 by 2000. Analysts have explained Cuba’s health results in the face of adversity by pointing to several factors. During the worst years of the crisis, the health status of the population remained a fundamental government priority. In fact, the Cuban parliament increased the health sector budget in Cuban pesos and the share of GDP earmarked for health care at the expense of spending for the military and state administration. At the same time, the health sector hard currency budget was forced down by two-thirds as a result of falling exports.
Although scarcities abounded, they were shared. The educational status of the Cuban population worked for continued hygiene measures and health education. Important medical resources were centralised and moved to where they were most critically needed.
The dedication of Cuban health professionals, working under the most stressful conditions, was indispensable for the Cuban population to emerge from the worst of the crisis with their health status essentially intact.
The health status of the population, vastly improved by the health care system since 1960, provided a sound foundation that could not be easily eroded. By the ’90s, Cuban children were being vaccinated against 13 childhood diseases – more than any other country in the world, including the United States. A host of diseases had been eradicated altogether, infectious diseases were at a minimum, and Cubans were dying of the same chronic conditions described in the mortality charts of industrialised countries. A significant socio-political corollary was that the majority of Cubans trusted the health care system to work for them.